Deep within the dark, almost oxygen-free recesses of the human gut lies an entire universe… of over 100 trillion gut microbiota.
These little guys outnumber our cells 10:1. (1)
Because they’re super tiny, they only make up about 1-3% of your body’s mass.
But that still means you’re carrying around 2-6 lbs of microbes on your person. (2)
There are 100,000 times more microbes in your gut alone as there are people on earth. (3)
These microbes include “good” and “bad” bacteria, fungi, viruses, and other single-celled organisms.
Together, they make up your gut microbiome.
Your microbiome is as unique as your fingerprint – no two people have the same microbiota makeup, in terms of bug strains and species.
“Microbes are barely separated from the gut’s immune cells and the numerous cellular sensors that encode our gut sensations… They live intimately in contact with the major information-gathering systems in the body.”
– Emeran Mayer, MD, author of: ‘The Mind-Gut Connection’
The health and diversity of your microbiome is determined by your genetic makeup, your mother’s microbiome state, your diet, your metabolism, age, geography, antibiotic usage history, stress, and your predominant mental and emotional state. (4)
Gut bacteria imbalances in your microbiome (aka dysbiosis) can negatively impact your quality of life and create mental health problems as well as a host of other health issues.
An imbalanced microbiome has been linked to mood disorders and mental illnesses like bipolar disorder, anxiety, major depressive disorder, and even autism spectrum disorder.
Having too much of the wrong kind of gut microbes in your digestive tract can also cause overactive immune activation because over 80% of your immune system is located in your gut.
The Gut-Brain Axis (GBA) – aka the Gut – Brain Connection:
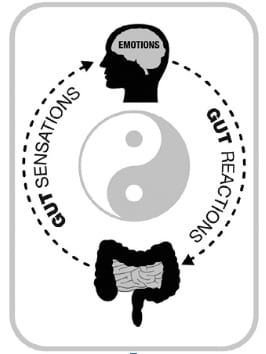
“In Chinese philosophy, the concept of yin and yang describes how opposite or contrary forces can be viewed as complementary and interconnected, and how they give rise to a unifying whole by interacting with each other.
When applied to the brain-gut axis, we can view our gut feelings as the yin, and gut reactions as the yang.
Just as yin and yang are the two complementary principles of the same entity— the brain-gut connection— both the feelings and the reactions are different aspects of the same bidirectional brain-gut network that plays such a crucial role in our well-being, our emotions, and our ability to make intuitive decisions.
– Emeran Mayer, MD, author of: ‘The Mind-Gut Connection’
You have a brain in your gut.
It’s called the Enteric Nervous System (ENS).
This Gut Brain is comprised of approximately 200-600 million neurons* located within the wall of your GI tract. (5)
The ENS functions like a supercomputer receiving and sending signals up to the Head Brain’s Central Nervous System (CNS), which is like the “central command station” for your body.
These two brains ‘talk’ and communicate with one another just like the diagram above shows.
Their conversation is comprised of a sort of ‘push and pull’ that resembles the yin-yang philosophy in Chinese medicine.
When one brain is out of whack, alert messages travel to the other brain and disrupt the collective flow.
Since the Gut-Brain is so intimately connected to your microbiome the GBA is also often referred to as the Microbiome-Gut-Brain Axis.
How Your Stress Impacts Your Digestive Health:
Stress is connected to our “fight/ flight/ freeze” response, which revs up our stress hormones and shuts down digestion in order for the body to preserve its energy for survival mode running or confronting.
If we’re chronically in “fight/ flight/ freeze,” especially when we eat, our digestive system is not able to operate at full capacity, creating sluggish, erratic food digestion, among many other complications, like bloating, gas, improper nutrient absorption, and acid reflux, which we saw was the most common digestive upset according to the Amino study.
That’s why the opposite of the “fight/ flight/ freeze” response is called the “rest and digest” response.
When we’re in a more relaxed state our digestive system gets the signal that it’s time to do its thing and optimize the entire digestive process – from mouth to booty hole.
It’s becoming very well known and more widely accepted that chronic anxiety is connected to chronic GI problems thanks to the growing amount of research.
For example:
- Irritable Bowel Syndrome (IBS) is ‘strongly associated’ with Generalized Anxiety Disorder (GAD) (6)
- Stress, especially prolonged stress, can create both short and long term effects on the functions of the GI tract thereby leading to the development of a “broad array of gastrointestinal disorders including inflammatory bowel disease (IBD), irritable bowel syndrome (IBS) and other functional gastrointestinal diseases, food antigen-related adverse responses (food allergies), peptic ulcer and gastroesophageal reflux disease (GERD).” (7)
The Gut Microbiome and Mental Health: Research
“We have discovered that the gut microbiota influences our emotions.
We have shown that people who are clinically depressed have less diversity in the bacteria in their gut than people who are not depressed.
The question now is how can we improve the diversity of our bacteria.”
– Dr. John Cryan, Ph.D., Professor & Chair of the Department of Anatomy and Neuroscience at the University College Cork
One study that examined the widespread presence of both IBS and GAD (Generalized Anxiety Disorder) found that out of 2005 participants:
GAD was five times more common among those with IBS than those without IBS.
They also found that IBS was 4.7 times more common among those with GAD.
The study concluded that IBS and GAD concurrence was common and “added to impairment in the community.” (8)
Another recent study conducted by gastroenterologist and researchers Dr. Premysl Bercik and Dr. Stephen Collins of Farncombe Family Digestive Health Research Institute at McMaster University jointly with the Department of Biology at the University of Waterloo found that transplanting fecal microbiota (gut bugs found in poop) from people with IBS alters gut function and behavior in recipient mice. (9)
The germ-free mice were implanted with poop from healthy guts as a control group, another group with poop from IBS patients with anxiety, and another group from non-anxiety IBS patients.
The mice implanted with poop from the IBS-anxiety patients resulted in faster GI transit, low-grade inflammation, and anxiety-like behavior. (9)
Further research by Drs. Bercik and Collins confirm that gut bacteria play an important role in inducing anxiety and depression.
They studied the role of intestinal microbes in behavior changes resulting from early life stress by separating newborn mice from their mothers for three hours/day from the time they were three days old until they were three weeks old. (I know, poor babies!) (10)
Now, what’s interesting is that you’re at a higher risk for gut issues if you experienced stress or trauma early on in life:
“Neonatal stress leads to increased stress reactivity and gut dysfunction that changes the gut microbiota which, in turn, alters brain function…
We show that relatively minor changes in microbiota profiles or its metabolic activity induced by neonatal stress can have profound effects on host behavior in adulthood.
It would be important to determine whether this also applies to humans.
For instance, whether we can detect abnormal microbiota profiles or different microbial metabolic activity in patients with primary psychiatric disorders, like anxiety and depression,” commented Dr. Bercik. (10)
How Your Gut Impacts Your Stress & Mood:
If you’re experiencing GI symptoms, chances are it will increase your stress levels and therefore your stress levels, especially if these symptoms are chronic and go on for a while.
If your symptoms are severe, say, there’s blood involved, or a lot of mucus, just the sight and thought of that can create psychological stress.
If you’re experiencing indigestion and heartburn, that pain and discomfort can intensify feelings of irritability and anxiety.
Trapped gas creates bloating, which definitely makes anyone feel uncomfortable.
Gas can also feel like pressure in the chest, which can trigger a panic or anxiety attack in some.
An upset belly can also create an imbalance in your gut flora (comprised of the bugs that live in your intestines, more on this in the sections to come.)
Imbalanced gut flora can lead to a slew of other problems like a domino effect.
If your gut tissues are particularly compromised, this can lead to poor nutrient absorption and poor nutrient production in your belly.
This leads to micronutrient deficiencies.
Certain micronutrient deficiencies have been linked to states of anxiety:
- “The most common nutritional deficiencies seen in patients with mental disorders are of omega–3 fatty acids, B vitamins, minerals, and amino acids that are precursors to neurotransmitters.” (11)
- Low Vitamin B6 and iron levels have also been linked to panic attacks and hyperventilation attacks. According to one study, they found that: “both Vit B6 and iron levels were significantly lower in the Panic Attack (PA) /Hyperventilation Attack (HVA) group than in the volunteer group,” in a study of 21 PA/HVA patients and comparing against 20 volunteers. (12)
Improve Gut Health & Mental Health With Psychobiotics:
“We defined a psychobiotic as a live organism that, when ingested in adequate amounts, produces a health benefit in patients suffering from psychiatric illness.
As a class of probiotic, these bacteria are capable of producing and delivering neuroactive substances such as GABA (gamma-aminobutyric acid) and serotonin, which act on the brain-gut axis.
Preclinical evaluation in rodents suggests that certain psychobiotics possess antidepressant or anxiety-reducing activity.
Effects may be mediated via the vagus nerve, spinal cord, and neuroendocrine systems.
Recently we have suggested broadening the psychobiotic concept to include prebiotics – the fiber that acts as food for the psychobiotics.”
– The Psychobiotic Revolution, by John Cryan & Ted Dinan
It’s wise to make it a priority to take a daily high-quality probiotic.
There are multiple ones on the market and not all of them as effective so be sure to discuss this with your doctor or health care provider.
Another thing you can do immediately is to start incorporating prebiotic-rich foods in your daily diet to ensure that you’re feeding the good gut bugs.
Here’s a list of 17 prebiotic-rich foods:
- garlic
- onions
- leeks
- asparagus
- barley
- bananas
- oats
- apples
- konjac root
- cacao
- flax seeds
- seaweed
- leafy greens
- jicama root
- dandelion
- Jerusalem artichoke
- chicory root
REFERENCES
:
(1) https://www.nih.gov/news-events/news-releases/nih-human-microbiome-project-defines-normal-bacterial-makeup-body
(2) http://ed.ted.com/on/akg9D3p6
(3) Emeran Mayer, MD, The Mind-Gut Connection, 2016
(4) http://neuroscienceresearch.wustl.edu/userfiles/file/Gut_brain%20axis%20How%20the%20microbiome%20influences%20anxiety%20and%20depression_Tran%20%20%20.pdf
(5) Martin-Merino, E., Ruigomez, A., Wallander, M., Johansson, S. and Garcia Rodriguez, L. (2009). Prevalence, incidence, morbidity and treatment patterns in a cohort of patients diagnosed with anxiety in UK primary care. Family Practice, 27(1), pp.9-16.
(6) https://www.ncbi.nlm.nih.gov/pubmed/19552631
(7) http://www.jpp.krakow.pl/journal/archive/12_11/pdf/591_12_11_article.pdf
(8) https://www.ncbi.nlm.nih.gov/pubmed/19552631
(9) http://stm.sciencemag.org/content/9/379/eaaf6397
(10) https://fhs.mcmaster.ca/main/news/news_2015/role_of_bacteria_in_anxiety_and_depression.html
(11) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2738337/
(12) https://www.ncbi.nlm.nih.gov/pubmed/23603926