If there’s one thing to know about the human body; it’s this: the human body has a ringmaster.
This ringmaster controls your digestion, your immunity, your brain, your weight, your health, and even your happiness.
This ringmaster is the gut
– Nancy Mure, author
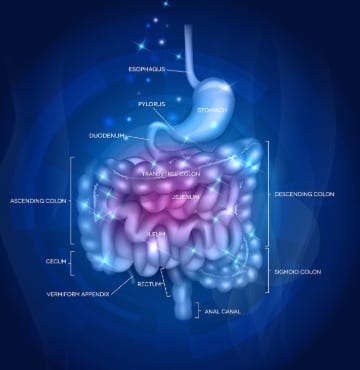
There within the dark internal folds of thegastrointestinal tractof thehumangutlies a whole other universe composed of over 100 trillion littlegut microbesthat make up what’s called yourgutmicrobiome.
These little microscopic critters play animportant rolein maintaining physical andmental health.
This is because we are in constant relationship with these little guys.
Our very functioning depends on them.
We have acommensal(non-harmful) relationship with ourgut bacteria.
And as with any relationship, harmony is needed in order to flourish.
Microbiomebalance is key if we’re to cultivate well-being because an imbalance in the gut (dysbiosis) can lead to an imbalance of the mind.
When the “good”microflora(bugs) outweigh the “bad” gut bugs we feel good and perform and think at our best.
When the “bad” bugs outweigh the “good” we often experienceanxiety-like behaviors, insomnia, weight gain, brain fog, declinedcognitive function, and compromised overallbrain function.
Since approximately 80% of theimmune systemis found in the gut we can also experience animmune responseand inflammation if our gut is imbalanced.
You not only have trillions of gut bugs living in your intestines, but you also possess a second brain in there too.
That’s right there’s a brain in your gut.
(And btw – there’s a brain in your heart too but we’ll save that for another time.)
Well, more specifically there’s an intelligent nervous system in your gut.
This Gut-Brain is in tight communication with the brain in your head and is also in close proximity to yourmicrobiome.
The system by which these three interact with each other is referred to as theMicrobiota-Gut-Brain Axis.
Gut-Brain Communication
The brain in your gut is called theEnteric Nervous System(ENS).
It’s comprised of approximately 200-600 million neurons* located within the wall of your GI tract. (1)
(*A neuron is an electrically excitable cell that sends and processes information through electrical and chemical signals.)
Gut-brain activity can influence head brain activity.
The ENS functions like a supercomputer receiving and sending signals up to the head brain’sCentral Nervous System(CNS), which is like the “central command station” for your body.
These two brains ‘talk’ and communicate with one another just like the diagram above shows.
Their conversation is comprised of a sort of ‘push and pull’ that resembles the yin-yang philosophy in Chinese medicine:

When one brain is out of whack, alert messages travel to the other brain and disrupt the collective flow.
The ENS contains more neurons than the spinal cord (2)
The ENS interacts with the CNS via theautonomic nervous system(ANS), and more specifically, via the parasympathetic nervous system (PSNS), mainly by way of theVagus Nervewhich is also known as Cranial Nerve X and runs from the base of your head through the face and middle ear, through the throat and heart, down to your gut.
Vagalactivity carries information from the gut to the head brain.
Jay Pasricha, M.D., director of the Johns Hopkins Center for Neurogastroenterology, has conducted internationally recognized research on the ENS.
He says:
“Its main role is controlling digestion, from swallowing to the release of enzymes that break down food to the control of blood flow that helps with nutrient absorption to elimination…
The enteric nervous system doesn’t seem capable of thought as we know it, but it communicates back and forth with our big brain—with profound results.” (3)
According to a Johns Hopkins Medicine report:
“The ENS may trigger big emotional shifts experienced by people coping withirritable bowel syndrome(IBS)and functional bowel problems such as constipation, diarrhea, bloating, pain and stomach upset.
Researchers are finding evidence that irritation in the gastrointestinal system may send signals to the central nervous system (CNS) that trigger mood changes.” (4)
To which Dr. Pasricha says:
“For decades, researchers and doctors thought that anxiety and depression contributed to these problems.
But our studies and others show that it may also be the other way around.
These new findings may explain why a higher-than-normal percentage of people withIBSand functional bowel problems develop depression and anxiety.
That’s important because up to 30 to 40 percent of the population has functional bowel problems at some point.” (4)
Gastrointestinal disorderslikeIBSandinflammatory bowel diseasecreate an increased risk for mental disorders like anxiety, panic attacks, and depression.
Interestingly enough, GI imbalance has also been linked to non-digestive disorders like Parkinson’s disease and Alzheimer’s disease. (5) (6)
There also seems to be a correlation between stress and trauma experienced in early life and the health of the microbiome and immune system. (6)
Stress and trauma can also changebrain developmentleading to impaired GBA function.
TheMicrobiome-Gut-Brain Axis(GBA):
This diagram represents the Microbiome – Gut-Brain Axis (GBA) and the various connections with these other big players like the immune system.
It’s extracted from a review titled: “Gut-Brain Axis: How the Microbiome Influences Anxiety & Depression,” conducted by researchers from the Department of Psychiatry & Behavioural Neurosciences at McMaster University:
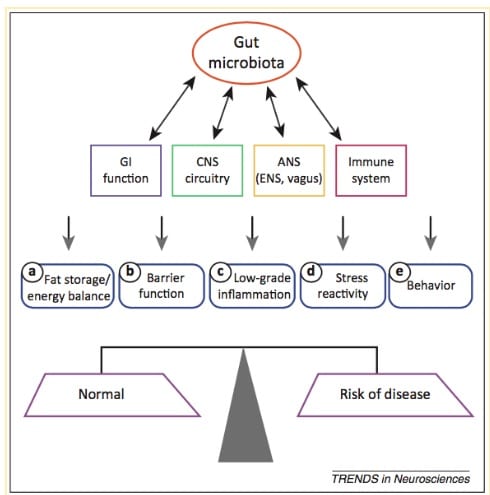
They explain:
“Bidirectional (two-way) communication betweengutmicrobiotaand components of thegut-brain axisinfluences normal homeostasis (balance) and may contribute to the risk of disease.
Alterations in gastrointestinal (GI), central nervous system (CNS), autonomic nervous system (ANS), and immunity systems by microbiota may lead to alterations in: (7)
(a) fat storage and energy balance
(b) GI barrier function
(c) general low grade inflammation (GI and systemic)
(d) increase stress reactivity
(e) increased anxiety and depressive-like behaviors.”
Microbiome-GBA is an integrated system.
Think of it as a supercomputer with an amazing capability to process, analyze, and store/retrieve gigantic amounts of information.
It links the emotional and thinking brain centers with the gut-brain and microbes.
The immune and hormonal systems play a role as well.
Gut hormonesare a major source of GBA communication.
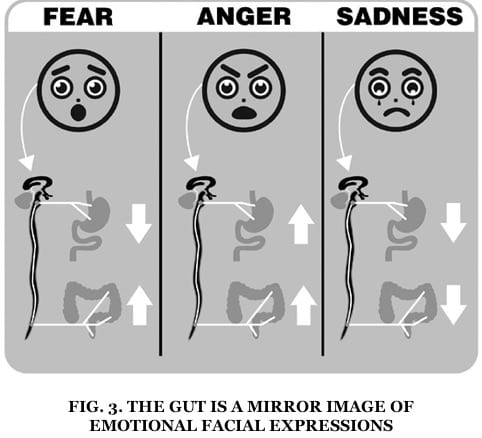
During periods of elevated or chronic stress/anxiety the brain’s emotional operating systems go on overload and send chaotic signals to the gut down below.
These signals create domino effects in your digestive system, which then, in turn, reacts and sends signals back up to the brain.
As Dr. Emeran Mayer explains in the Mind-Gut Connection:
“Expression of our emotions occurs in the different regions of the GI tract.”
The Physical Symptoms of Gut Imbalance:
Every day we live and every meal we eat we influence the great microbial organ inside us – for better or for worse.
– Giulia Enders, Gut: The Inside Story of Our Body’s Most Underrated Organ
All of this can alter yourmicrobiomeenvironment/habitat.
For your gut bugs, these environmental changes are similar to big global climate shifts, except that it’s happening in the microworld of your insides.
It’s like the Butterfly Effect of chronic stress and your gut converging.
One little crease or crack, repeated with intensity and consistency, can lead to big changes over time.
Before you know it, your chronic anxiety, underlying overwhelm, and unresolved emotional charges manifest in your physical body as symptoms:
- Yourimmune systemis compromised or overactive.
- You develop food sensitivities.
- You start experiencing digestive problems like gas, acid reflux, constipation, diarrhea, bloating, belching, and abdominal cramps.
- Your body’s toxic load increases.
- You get sick easier.
- You experience inflammation in some form, whether you’re aware of it or not.
- Your joints start to ache.
- You get headaches more frequently.
- You often feel tired and moody.
- You suddenly gain or lose drastic weight.
- You can’t focus or remember things.
- Your mojo is nowhere to be found – libido down.
All of these symptoms are feedback.
They are the ways in which your body and all its systems are talking to you, trying to get your attention, trying to bring you back to center and back to homeostasis (balance).
Your Gut & YourStress Response:
The ENS/ Gut-Brain also interacts with theneuroendocrinesystem (nervous system <– neuro / endocrine –> hormones) by way of theHPAAxis.
The HPA (Hypothalamic-Pituitary-Adrenal) Axis is where your nervous system and hormonal system intersect to create a cascading symphony of signals, feedback, and chemicals in response to any perceived stress or danger.
This results in stress hormones circulating in your bloodstream.
Three endocrine (hormonal) glands are involved in this process:
1. The Hypothalamus (aka: the Master Gland, the Boss)
2. The Pituitary gland (does what the Hypothalamus tells it to do)
3. The Adrenal glands (they sit atop the kidneys)
Stress responseactivation andHPA Axisactivity results in the production of a hormone called CRF (Corticotropin-Releasing Factor).
Dr. Yvette Tache has conducted groundbreaking research on the role of CRF in stress-related alterations of theGut-Brain Axis.
Her work is exceptionally important because it links gut dysfunctions likeIBS(Irritable Bowel Syndrome) and IBD (Inflammatory Bowel Disease) to thestress response.
Improve Gut Health &Mental HealthWithPsychobiotics:
We defined a psychobiotic as a live organism that, when ingested in adequate amounts, produces a health benefit in patients suffering from psychiatric illness.
As a class ofprobiotic, these bacteria are capable of producing and delivering neuroactive substances such asGABA(gamma-aminobutyric acid) and serotonin, which act on thebrain-gutaxis.
Preclinical evaluation in rodents suggests that certainpsychobioticspossess antidepressant or anxiety-reducing activity.
Effects may be mediated via thevagus nerve, spinal cord, andneuroendocrinesystems.
Recently we have suggested broadening the psychobiotic concept to include prebiotics – the fiber that acts as food for the psychobiotics.
– ThePsychobioticRevolution, by JohnCryan& TedDinan
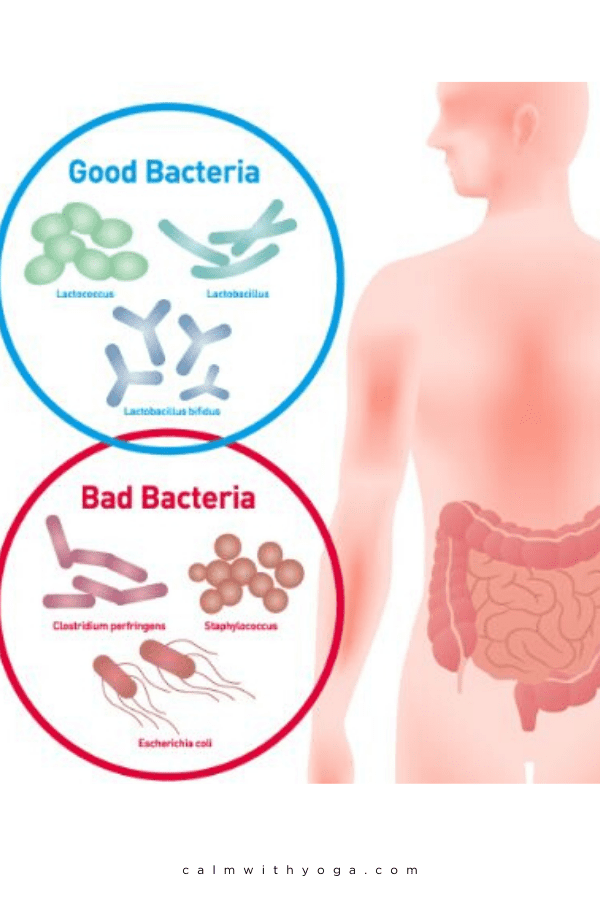
There are two kinds of intestinal microbiota in the gut – the good ones that help our bodies function properly and the ones that harm us and create dis-ease. (8)
Common “good” gut bugs are lactic acid bacteria, bifidobacterium, and lactobacillus for example.
A common strain of “bad” bacteria (aka enterobacteria) isclostridium.
“Bad” bacteria contain a toxin calledlipopolysaccharide(LPS) within the bacterial cell.
Because of thismicrobiotacompositionLPScan be a major cause for inflammation and theimmune responsein us humans.
Probiotics:
Probioticsare live bacteria cultures. (Essentially, gut bugs.)
When we ingest these little guys a good amount of them reach the intestine in an active state and promote multiple beneficial health benefits, like helping keep yourmicrobiomebalanced so that there is no overgrowth of detrimental bacteria that can lead to infections and other health problems.
Probioticshave also been shown to interact directly with theimmune system, helping to reduce gut inflammation and reducing the body’s stress levels. (9)
Not having enough probiotics in the gut can lead to imbalances of the microbiome, which has been linked to GI conditions like inflammatory bowel diseases (IBD) like Crohn’s Disease and Ulcerative Colitis, irritable bowel syndrome (IBS), and even obesity, and type 2 diabetes. (10)
Prebiotics:
Prebioticsaren’t living organisms likeprobiotics; they’re a substance that comes from fermentable fibers that we eat but cannot digest.
Prebioticsare essentially food for theprobioticsin our gut.
Probiotics eat prebiotics and then ferment what’s left into what are called short-chain fatty acids (SCFA’s.)
This process releases the neurotransmitter serotonin and anti-inflammatory agents which reduce stress signals to the brain. (10)
Although more research is needed, it certainly does appear that regular consumption of both pre and probiotics can help regulate our hormones and therefore regulate our mood. One study out of Oxford University found that consumption of prebiotics can significantly impact the brain, lowering stress hormone (cortisol) levels and therefore lower the body’s stress response and anxious tendencies. (11)
Gut bacteriaproduce hundreds ofneurochemicalsthat are used by the brain to regulate body function and mood.
Did you know thatgut bacteriaproduce around 95% of the body’s serotonin supply?
Serotonin is a neurotransmitter thought to be a contributor to feelings of well-being and happiness.
Serotonin is made from the essential amino acidtryptophanfound in foods such as eggs, meat, legumes, and poultry.
It’s hypothesized that eating a diet rich in this amino acid is then metabolized by the gut bugs which leads to the production of molecules that are beneficial to our physical and mental health. (12)
Gut bacteriaalso play a big role in increasing levels of BNDF (brain-derivedneurotrophic factor) which acts like fertilizer or growth hormone for the brain.
Some experts such as Dr. David Perlmutter believe that the right probiotic supplementation can stimulate BDNF thereby promoting neurogenesis (growth of new brain cells). (13)
REFERENCES
:
(1) https://www.ncbi.nlm.nih.gov/pubmed/24997029
(2) https://www.scientificamerican.com/article/gut-second-brain/
(3) http://www.hopkinsmedicine.org/health/healthy_aging/healthy_body/the-brain-gut-connection
(4) https://www.scientificamerican.com/article/does-parkinsons-begin-in-the-gut/
(5) http://www.jnmjournal.org/view.html?uid=1449&vmd=Full
(6)SudoN, Chida Y, Aiba Y, Sonoda J, Oyama N, Yu XN et al (2004) Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system forstress responsein mice.J Physiol558(Pt 1):263–275, PubMed PMID: 15133062, Pubmed Central PMCID: 1664925, Epub 2004 May 7
(7) http://neuroscienceresearch.wustl.edu/userfiles/file/Gut_brain%20axis%20How%20the%20microbiome%20influences%20anxiety%20and%20depression_Tran%20%20%20.pdf
(8) Kennedy EA, King KY, Baldridge MT. MouseMicrobiotaModels: ComparingGerm-Free Miceand Antibiotics Treatment as Tools for ModifyingGut Bacteria.Front Physiol. 2018;9:1534. Published 2018 Oct 31. doi:10.3389/fphys.2018.01534
(9)https://www.ncbi.nlm.nih.gov/pubmed/18461293
(10)https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4566439/
(11) https://wholefoodsmagazine.com/supplements/features-supplements/pre-probiotics-thinking-outside-gut/
(12) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4410136/
(13) https://www.drperlmutter.com/gut-bacteria-bdnf/